Ruth was 79 years old when she was diagnosed with early stage I breast cancer in 2018. A breast lump had been found on a routine examination.
A biopsy later confirmed breast cancer. Further testing confirmed that the surface of her cancer cells was covered with a protein called HER2. The presence of HER2 protein on the cancer cells indicated a more aggressive form of breast cancer with a higher recurrence rate. Fortunately, there was an effect therapy for HER2+ breast cancer. Ruth’s oncologist wanted her to receive Herceptin (trastuzumab), an immune therapy shown to improve survival and decrease cancer recurrence. After undergoing a lumpectomy to remove the cancer, her oncologist prescribed treatment with from Herceptin and Taxol, a chemotherapeutic agent.
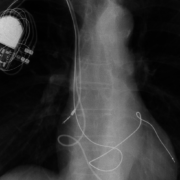
Before starting Herceptin, Ruth had an echocardiogram, which is an ultrasound study to evaluate the heart pump function. Unfortunately Ruth’s echocardiogram showed that her heart heart function was moderate to severely reduced. One of the potential side effects of Herceptin was a weakening of the heart pump, which can cause congestive heart failure. She was therefore referred to the  Cardio-Oncology Clinic at MHVI. Ruth’s cardiologist decided that she could improve her heart function with the use of a special pacemaker, called a biventricular pacemaker. This pacemaker was designed to improve heart function in patients with a low heart function and certain electrical conduction defects. A biventricular pacemaker was successfully placed in Ruth (see x-ray). A follow-up echo showed that her ejection fraction had improved enough to start treatment with Herceptin. She was followed closely in the Cardio-Oncology Clinic while receiving cancer treatment and in the end completed 6 months of therapy with Taxol and Herceptin with no signs of additional weakening of the heart function. Throughout her course of chemotherapy, Ruth was able receive cancer treatment with minimal damage to her heart. Now, more than two years later she is doing well. Ruth is able to play with her grandkids, attend church, and she remains cancer-free.
Cardio-Oncology Clinic at MHVI. Ruth’s cardiologist decided that she could improve her heart function with the use of a special pacemaker, called a biventricular pacemaker. This pacemaker was designed to improve heart function in patients with a low heart function and certain electrical conduction defects. A biventricular pacemaker was successfully placed in Ruth (see x-ray). A follow-up echo showed that her ejection fraction had improved enough to start treatment with Herceptin. She was followed closely in the Cardio-Oncology Clinic while receiving cancer treatment and in the end completed 6 months of therapy with Taxol and Herceptin with no signs of additional weakening of the heart function. Throughout her course of chemotherapy, Ruth was able receive cancer treatment with minimal damage to her heart. Now, more than two years later she is doing well. Ruth is able to play with her grandkids, attend church, and she remains cancer-free.
Ruth’s story highlights one of the main goals of the Cardio-Oncology Clinic at MHVI. We work closely with cancer patients and their cancer specialists to help patients receive optimal cancer therapy while trying to prevent or minimize cancer related heart toxicity and symptoms.
>> Learn more about Cardio-Oncology Clinic
>> Learn more about Biventricular Pacemaker (Cardiac Resynchronization Therapy)


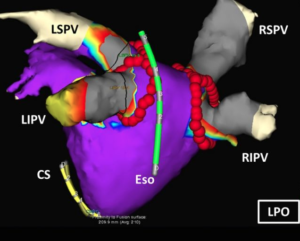 Eventually Joan retired, but she felt like she was being robbed of a peaceful retirement due to the endless ER visits, sleeping difficulties and constant fear of going back into an irregular rhythm. In April 2008, after 12 years of battling her heart rhythm condition, Joan underwent catheter ablation for atrial fibrillation (also known as
Eventually Joan retired, but she felt like she was being robbed of a peaceful retirement due to the endless ER visits, sleeping difficulties and constant fear of going back into an irregular rhythm. In April 2008, after 12 years of battling her heart rhythm condition, Joan underwent catheter ablation for atrial fibrillation (also known as 
 Eventually, Patricia’s heart pump weakened to the point where she could barely walk into clinic from her car to see her doctors. She needed to ride a cart just to do grocery shopping. Previously an independent woman, she increasingly relied on her daughter to do simple chores for her at home. Finally, five years after her diagnosis of heart failure, she agreed to receive a biventricular pacemaker-defibrillator. Dr. Joseph Lin, an MHVI heart rhythm specialist, performed this implant at Mercy Hospital. Within months, Patricia’s heart responded to the pacing and her heart pumped more efficiently. It went from being severely reduced in function to normal function. Looking back, Patricia says, “I should have listened to Dr. Kraemer and had this done sooner. I feel wonderful now. She reported recently, “My energy level has improved. I am doing my house chores.” She boasts, “I am very active socially.”
Eventually, Patricia’s heart pump weakened to the point where she could barely walk into clinic from her car to see her doctors. She needed to ride a cart just to do grocery shopping. Previously an independent woman, she increasingly relied on her daughter to do simple chores for her at home. Finally, five years after her diagnosis of heart failure, she agreed to receive a biventricular pacemaker-defibrillator. Dr. Joseph Lin, an MHVI heart rhythm specialist, performed this implant at Mercy Hospital. Within months, Patricia’s heart responded to the pacing and her heart pumped more efficiently. It went from being severely reduced in function to normal function. Looking back, Patricia says, “I should have listened to Dr. Kraemer and had this done sooner. I feel wonderful now. She reported recently, “My energy level has improved. I am doing my house chores.” She boasts, “I am very active socially.”

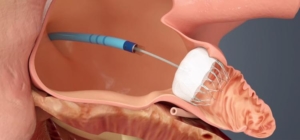 Due to her high risk for stroke and equally high risk for bleeding while taking blood thinners, her cardiologists at MHVI referred her to have a Watchman device implanted. This device was performed by MHVI specialists Dr. Joseph Lin and Dr. Jeffrey Chambers, who inserted it through a vein in her leg and steered it up to her heart. They deployed it to plug up a small pouch in the heart called the left atrial appendage, where blood pools and forms clots that can break off and cause strokes. The procedure took an hour to do and Sandra was discharged home the next day.
Due to her high risk for stroke and equally high risk for bleeding while taking blood thinners, her cardiologists at MHVI referred her to have a Watchman device implanted. This device was performed by MHVI specialists Dr. Joseph Lin and Dr. Jeffrey Chambers, who inserted it through a vein in her leg and steered it up to her heart. They deployed it to plug up a small pouch in the heart called the left atrial appendage, where blood pools and forms clots that can break off and cause strokes. The procedure took an hour to do and Sandra was discharged home the next day.



 “The data is real time and easy to interpret. We are able to intervene at least two weeks before patients actually start feeling the symptoms,” said Dr. Rahmatullah. Pulmonary artery pressure increases appear before weight and blood pressure changes, which are often used as indirect measures of worsening heart failure. Based on the sensor readings, his heart failure doctors and nurses adjust Del’s medications.
“The data is real time and easy to interpret. We are able to intervene at least two weeks before patients actually start feeling the symptoms,” said Dr. Rahmatullah. Pulmonary artery pressure increases appear before weight and blood pressure changes, which are often used as indirect measures of worsening heart failure. Based on the sensor readings, his heart failure doctors and nurses adjust Del’s medications.